How much do you know about the menopause?
If you’re 40 and suffer from anxiety, hot flushes, weight gain or sleep issues the likelihood is you have begun your transition to menopause already.
All menstruating women go through the menopause, it is not a disease or something to be ashamed of. Usually, it occurs between the ages of 45 and 55- in the UK the average age is 51, however 1 in 100 women can experience the menopause before they are 40.
The whole process can be very confusing mainly due to the fact:
1. Terminology is unclear – what actually is the menopause, perimenopause and post-menopause?
2. Information is limited and there is a lack of support and understanding.
3. It is a subject we’re reluctant to talk about – possibly because it is related to getting old.
Facts about the transition…
Approximately 13 million women in the U.K are either peri- or post menopausal.
Over 60% of women experience debilitating symptoms which can last up to 15 year.
Women commonly complain of feeling as though they are going mad, 1/2 of menopausal women say they feel depressed, 1/3 of women say they suffer with anxiety.
1 in 5 take time off work to deal with menopausal symptoms and 1 in 50 are on long term sick leave.
Is it any wonder we live in fear of the menopause transition?
As if the ageing process wasn’t bad enough, the symptoms of menopause have been at the centre of jokes about or used to depict women of a ‘certain age’ in the media and we have heard female friends discuss them with a sense of frustration, embarrassment or even sadness. This might have created a sense of fear for you around a stage in life that all menstruating women will transition through.
On top of this, seeking support can also be difficult.
About 38 per cent of women seek help from a GP but it is common they are incorrectly diagnosed as depressed and given antidepressants. A quarter of those who visited a GP say the possibility of the symptoms being menopause related is missed.
You know the menopause is unlikely to be plain sailing, nothing about female hormones is particularly pretty (you have had to deal with a monthly bleed the majority of your life for goodness sake). BUT it is a natural process, one that ‘bodies with ovaries’ have been going through since the beginning of time and so you need to try and embrace the privilege of ageing.
As life expectancy increases and attitudes to ageing evolves, people are starting to see menopause as a new beginning rather than an end. There is so much life, love and living after menopause and you need to feel empowered to enjoy every minute of it.
Knowing what to expect can help you feel empowered and make the transition simple.
Here are some things you need to know…
Menopause Basics
The Menopause is the ceasing of your period due to low hormone levels and is defined as exactly 12 months since your last period.
Peri-menopause means "around menopause" and refers to the time during which your body makes the natural transition to menopause, marking the end of the reproductive years. Peri-menopause is also called the menopausal transition.
The ‘peri-menopause’ starts as early as your 30’s and on average continues for 10 years.
Post menopause is the time after ‘12 months without a period’. Symptoms continue for approximately 4-5 years but they decrease in frequency and intensity.
How do sex hormones help us?
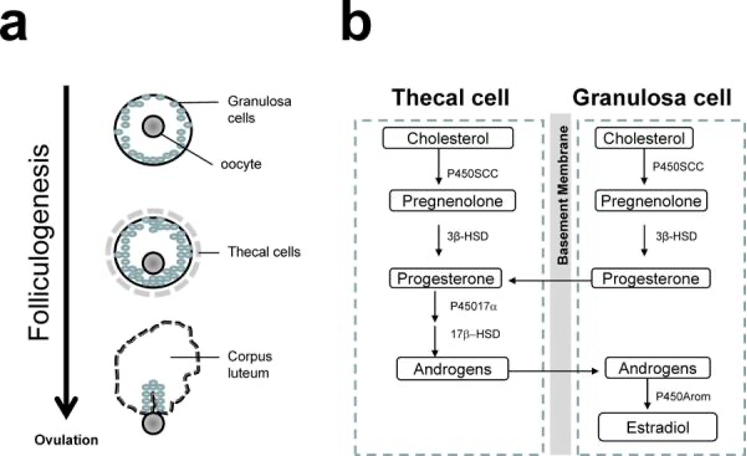
Oestrogen and progesterone are steroid hormones that play a pivotal role in the regulation of reproduction. Their primary function is to regulate the development and function of the uterus. However, they have far more health benefits than you may realise.
Oestrogen’s role
There are 3 oestrogen hormones. The ovaries, produce oestradiol (E2) which is the most common type of oestrogen during your reproductive years.
Oestrogen plays an important role in various essential functions like:
sexual desire and sexiness
lipid metabolism
brain function
bone health
skin health
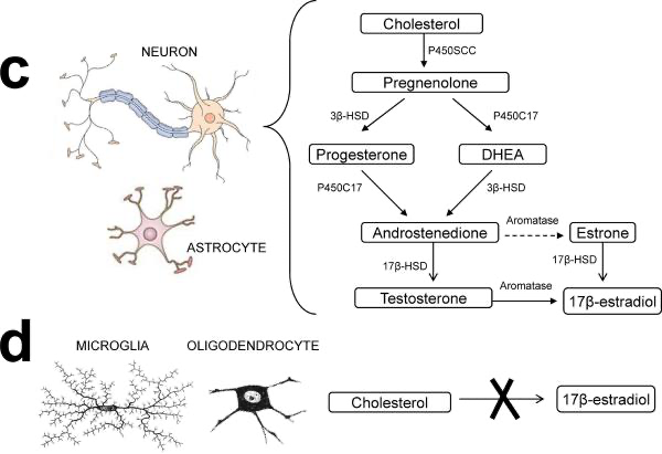
Although oestrogen lowers during the menopause, it’s important to know that the body does not stop producing it completely. Instead of being created by the ovaries, the adrenal glands and adipose fat tissue form hormones called androgens, and aromatase converts them into oestrone (E1), the second oestrogen. This is a weaker form but one the body can convert to other forms of oestrogen, as necessary.
These images show the different cells involved and pathways to hormone production.
Cui, J., Shen, Y. and Li, R., 2013. Estrogen synthesis and signalling pathways during ageing: from periphery to brain. Trends in molecular medicine, 19(3), pp.197-209.
Oestriol (E3) is the third oestrogen. It rises during pregnancy, as it helps the uterus grow and prepares the body for delivery.
How does the peri-menopause affect your body?
When the perimenopause starts, your ovaries begin to falter and stammer. They lose control of the wheel and lurch from over-production of oestrogen and progesterone to not making enough. These big fluctuations result in a severe hormone rollercoaster, with mood swings to match. They make testing and medicating incredibly challenging. Not only that but the loss of hormones can be a meandering descent over years or be a plummeting crash.
For this reason, the peri-menopause can be challenging for you. A feeling of losing yourself, your confidence, feelings of irritability or tearfulness or rage which is abrupt and shocking. You may experience PMS symptoms such as breast tenderness, weight gain, bloating and poor sleep – while others describe an anxiety which is new and utterly debilitating.
You may experience symptoms that range from mild to severe.
Common symptoms include:
Hot flashes: Sudden sensations of heat in the upper body affect up to 75% of people.
Night sweats: These are hot flashes that occur at night.
Difficulty sleeping: Night sweats, mood changes, and anxiety can make it hard to sleep.
Menstrual problems, such as light or heavy bleeding, (PMS),
Fatigue: oestrogen, progesterone, thyroid and adrenal hormones are involved in regulating cellular energy within the body. When they're out of balance, you may feel exhausted or fatigued for no particular reason.
Mood changes: Fluctuating hormone levels and environmental factors can contribute to stress, anxiety, and depression.
Hormonal changes can also contribute to osteoporosis. When a person has osteoporosis, their bone density decreases, and bones are more likely to break. The risk of osteoporosis rises during and after menopause.
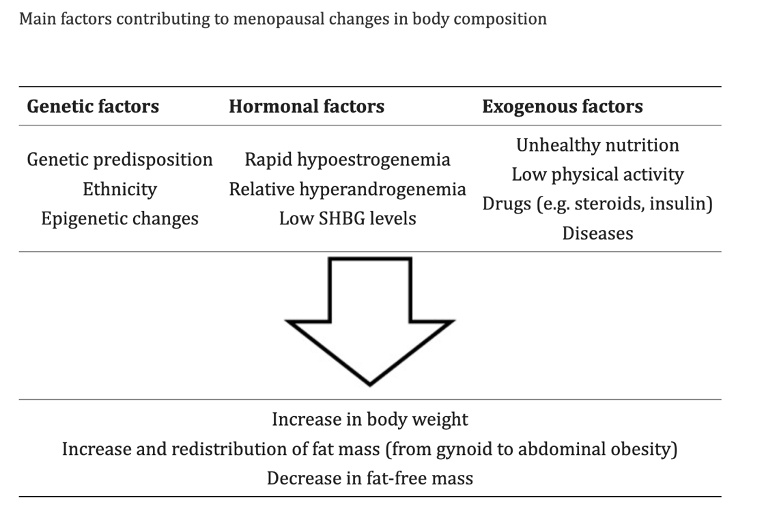
Weight gain: According to a 2017 article by J Proietto, most people experience some weight gain around menopause typically caused by hormonal, genetic and environmental factors (including metabolic disorders and stress) see table below.
Kozakowski, J., Gietka-Czernel, M., Leszczyńska, D. and Majos, A., 2017. Obesity in menopause–our negligence or an unfortunate inevitability?. Menopause Review/Przegląd Menopauzalny, 16(2), pp.61-65.
In addition, you may also begin to experience changes like;
vaginal dryness: sex can be painful as a result.
reduced libido: sexual desire can fall as hormone levels drop, but vaginal dryness can also make sex uncomfortable.
urinary tract infections
acne
constipation
fibrocystic breasts (non-cancerous breast lumps),
fibroids (noncancerous tumors) in the uterus,
breast swelling and tenderness
menstrual migraine, is a bad headache right before your period, due to the drop in oestrogen.
The main health concerns associated with menopause are those impacting your heart, brain and bones.
Heart - As oestrogen helps to control levels of cholesterol, during the decline the risk of fatty build up in the artery walls can lead to an increased risk of heart attacks.
Brain - The ‘brain fog’ often associated with menopause is often an early sign as it can come as a result in the initial dip in progesterone. This, alongside the changes in the balance of other hormone levels, is a key factor leading to the disruption in sleep patterns which can also impact memory. A study in 2018 by L Mosconi suggests there is an increased risk of Alzheimer’s in women of menopausal age. In general, you may feel lost for words, confused or irritable. Stress is a compounding factor which some call “brain fog.” Stress is a significant modifiable factor to consider here especially as the adrenals come under greater pressure to create hormones.
Bones - As oestrogen also plays a vital role in maintaining bone density, drops in these levels can lead to Osteopenia (lower than usual bone density) or Osteoporosis (a disease meaning that your bone density is so low that your bones are brittle and can break easily), both of which can cause concern about breaking bones.
What about HRT?
While studies suggest Hormone Replacement Therapy (HRT) is likely safe and may reduce risks of osteoporosis, cardiovascular disease, and for some give relief from severe symptoms. The effects and safety vary depending on the type of HRT used and how long you take it for, as well as your own personal health, including your genetics, family history of cancer, body mass index and liver health. One size does not fit all and most importantly the environment you add HRT to is as crucial as the hormones themselves.
Thankfully, risks and symptoms can also be alleviated by ensuring that your diet and way of life contribute to overall healthy function. If you want to know the BEST nutrition habits to relieve symptoms of the menopause.
Get FREE access to 5 nutrition hacks here…